Portal de la investigación

Este portal es un sistema de información que permite explorar la estructura de la I+D+i, localizar expertos en un campo de investigación científica y acceder a los resultados de la investigación que se desarrolla en La Universidad de La Rioja. Además es el repositorio institucional.
1.503
Proyectos
Hallado un nuevo biomarcador de diagnóstico y pronóstico del cáncer colorrectal
La Universidad de La Rioja participa en un proyecto de investigación, junto al CIBIR y el Hospital Universitario San Pedro, que ha logrado identificar un nuevo biomarcador para diagnosticar y predecir la supervivencia en pacientes de cáncer colorrectal
2024-03-26
«En un tiempo caracterizado por la incertidumbre, los problemas a los que nos enfrentamos sólo podrán ser superados con más y mejor ciencia»
El Doctor ‘Honoris Causa’ Javier García Martínez recibe de Sus Majestades los Reyes de España el Premio Nacional de Investigación ‘Juan de la Cierva’ en Gandía
2024-03-15
“Con la emergencia de la Inteligencia Artificial la sociedad se está dando cuenta de los problemas que presenta la tecnología”
ETHICOMP 2024 reúne a expertos de todo el mundo que abordan el impacto ético y social de las TIC y el “lado oscuro de la tecnología en la Universidad de La Rioja
2024-03-14
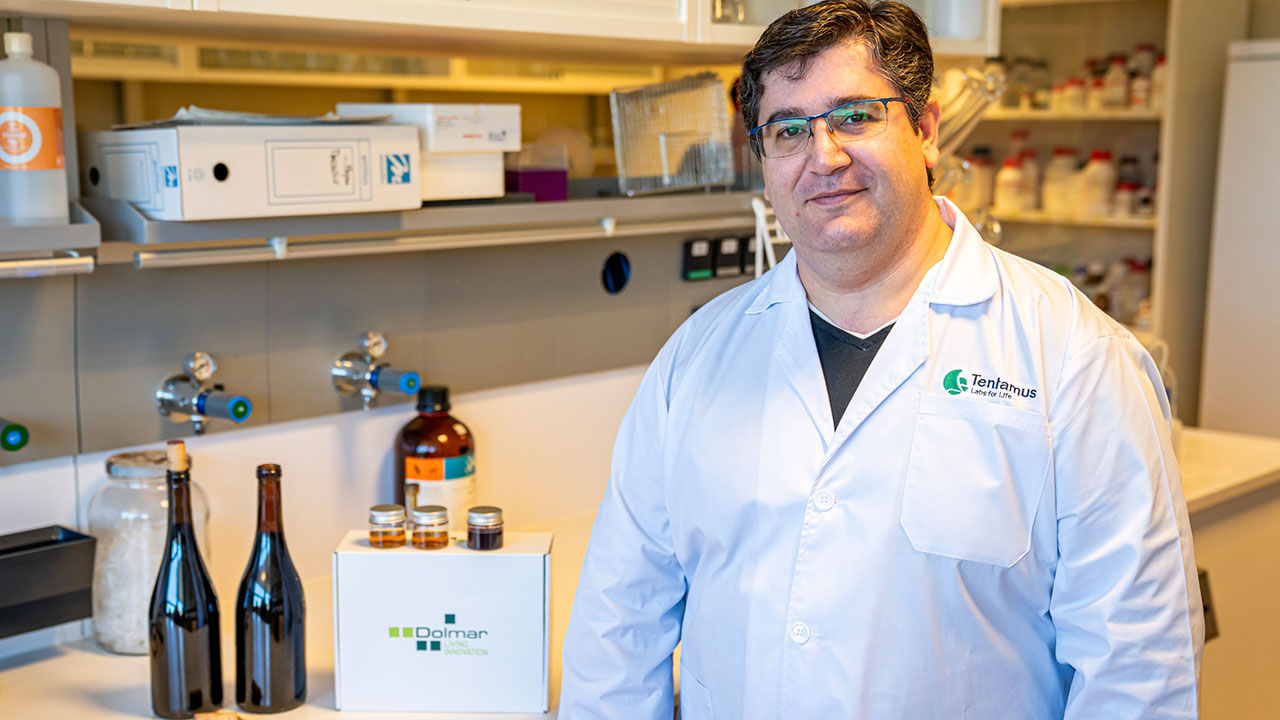
Un método permite detectar la cantidad de bacterias acéticas en el vino adelantándose a los aumentos que lo pican o avinagran
Alejandro Parra Manzanares se doctora con una tesis que desarrollo este método no patentado y, por tanto, a disposición de bodegas y viticultores
2024-03-05
Inés Soldevilla obtiene el grado de doctora con una tesis sobre nuevos compuestos de oro
La doctora da en su tesis los primeros pasos para lograr moléculas que mejoren las pantallas de dispositivos electroluminiscentes, como los empleados en las televisiones, ordenadores y teléfonos móviles
2024-02-19
“Hemos conseguido un biosensor que permite detectar el cáncer de próstata, ahora el objetivo es diseñar un prototipo”
El catedrático Francisco Corzana y el doctorando Víctor Pozo explican en una actividad de UR Saludable sus proyectos financiados por la Asociación Española contra el Cáncer (AECC)
2024-02-14
Investigadoras de la UR participan en un proyecto europeo sobre resistencia a los antimicrobianos
Carmen Torres Manrique, Myriam Zarazaga Chamorro, Carmen Lozano Fernández y Beatriz Robredo Valgañón están involucradas en el consorcio EU-JAMRAI 2, que aúna a 120 organizaciones de 30 países
2024-02-13
Glycopep4Life desarrolla una nueva vacuna contra el cáncer que genera una alta respuesta inmunitaria en ratones
La revista científica 'Journal of American Chemistry Society-Au' (JACS-Au) publica en abierto el hallazgo, que forma parte del proyecto DIRNANO financiado por la Comisión Europea
2024-02-02
La OTRI organiza una Jornada de presentación de la Convocatoria de Colaboración Público–Privada 2023
La Sala de Grados del Edificio Politécnico acoge el martes 23 de enero una jornada sobre la convocatoria de la Agencia Estatal de Investigación, dirigida a investigadores y empresas, con entrada libre
2024-01-18
Una tesis analiza 1.200 cepas de Staphylococcus en la búsqueda de alternativas a los antibióticos contra las bacterias resistentes
Rosa Fernández Fernández obtiene el grado de doctora con una tesis que estudia la producción de péptidos antimicrobianos como potencial alternativa a los antibióticos en el sector biomédico y agroalimentario
2024-01-17